Arthritis is a medical condition specifically targeting the joints, the points where bones come together and enable movement.
Typically, it leads to inflammation or deterioration of these joints, resulting in pain and discomfort during joint usage.
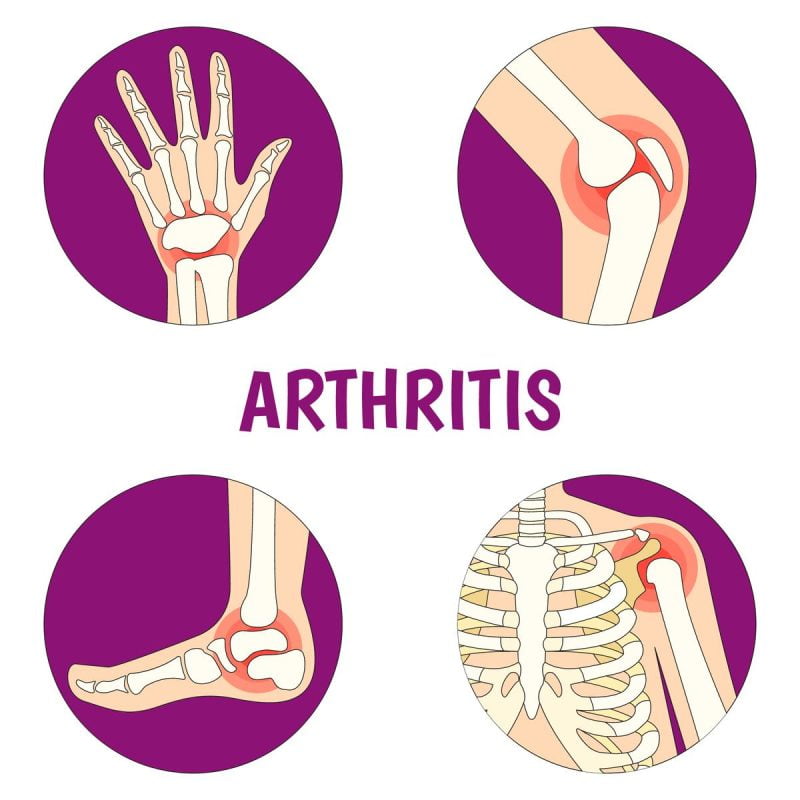
The most prevalent regions affected by arthritis are:
- Feet
- Hands
- Hips
- Knees
- Lower back
In these areas, the symptoms of it tend to manifest more frequently, causing discomfort and hindering mobility for individuals suffering from the condition.
What are the parts of a joint?
Soft tissues are vital in cushioning and supporting our joints, preventing bone-on-bone friction and discomfort. Among these soft tissues, the articular cartilage is particularly important, enabling smooth and painless movement of the joints.
In certain joints, a synovial membrane exists, acting as a cushioned pocket filled with fluid that lubricates the joints, further enhancing their functionality. Additionally, numerous joints, like the knees, are supported by tendons and ligaments.
Tendons connect muscles to bones, while ligaments connect bones to other bones, providing stability and facilitating coordinated movement within the joint structure.
What are the different types of arthritis?
Arthritis encompasses many joint conditions, with more than 100 different types identified. Some of the more prevalent types include:
Osteoarthritis
Also known as “wear and tear” arthritis, occurs when the joint cartilage deteriorates due to repetitive stress. Arthritis of this nature is by far the most prevalent.
Ankylosing spondylitis
Affecting the spine, typically the lower back; this form of arthritis causes inflammation and stiffness.
Juvenile arthritis (JA)
A disorder where the immune system targets the tissue surrounding joints. JA primarily affects children aged 16 or younger.
Gout
This condition leads to the formation of hard uric acid crystals in the joints, causing severe pain and inflammation.
Psoriatic arthritis
This involves joint inflammation in individuals with psoriasis, an autoimmune disorder that causes skin irritation.
Rheumatoid arthritis
An autoimmune disease that triggers the immune system to attack the synovial membranes in the joints, leading to inflammation and damage.
How usual is arthritis?
Arthritis stands as the leading cause of disability in the United States, affecting a significant number of individuals. U.S. households currently include approximately 50 million adults and 300,000 children. grapple with various forms of arthritis, impacting their daily lives and mobility.
What causes arthritis?
Various forms of arthritis stem from distinct causes. For example, gout is triggered by excess uric acid in the body. However, the precise causes of other types of arthritis remain unknown.
Individuals may develop it due to various factors, such as having a family history of the condition, engaging in jobs or sports that impose repetitive stress on the joints, or having certain autoimmune diseases or viral infections.
Each case of arthritis presents unique complexities that researchers continue to explore for better understanding and management.
What are the risk factors for arthritis?
Certain factors can heighten your susceptibility to developing arthritis. As you age, the risk of it escalates, making it more prevalent among older individuals.
Lifestyle choices significantly influence it’s risk, with smoking and a sedentary lifestyle increasing the likelihood of its occurrence.
Moreover, gender plays a role, as most types of arthritis are more commonly found in women. Maintaining a healthy weight is also crucial, as obesity places additional strain on your joints, which may lead to the development of arthritis.
Being aware of these risk factors and consciously adopting a healthy lifestyle can reduce the chances of experiencing it’s related issues.
What are the symptoms of arthritis?
Various types of arthritis exhibit diverse symptoms, and their severity can vary significantly from one person to another. Joint discomfort may range from mild to severe and can be intermittent or persistent.
The commonly observed symptoms encompass
- pain
- redness
- stiffness
- swelling
- tenderness
- Warmth in the affected areas.
These manifestations serve as crucial indicators when diagnosing the specific type of arthritis and tailoring appropriate treatment plans to address the individual’s unique needs. Regular monitoring of these symptoms can aid in managing it effectively and enhance the quality of life for those affected.
How is arthritis diagnosed?
If you suspect that you might be experiencing arthritis-related symptoms, seeking guidance from your healthcare provider is essential. During the consultation, your provider will inquire about your symptoms and how joint pain impacts your daily life.
A thorough physical examination will also be conducted, encompassing assessments of joint mobility and range of motion and checks for areas of tenderness or swelling around the affected joints. Moreover, your overall health will be evaluated to rule out other potential conditions contributing to your symptoms.
These evaluations and discussions are crucial in accurately diagnosing it and formulating an appropriate treatment plan tailored to your needs.
Can imaging exams detect arthritis?
Advanced medical imaging plays a vital role in providing your healthcare provider with comprehensive insights into your bones, joints, and soft tissues.
By utilizing X-ray, MRI, or ultrasound scans, your healthcare professional can uncover various essential aspects, including:
- Identifying bone fractures or dislocations that could be the underlying cause of your joint pain.
- Assessing the condition of the cartilage surrounding your joints, detecting any potential breakdown or damage.
- Evaluating muscle, ligament, or tendon injuries near your joints, aiding in accurate diagnosis and treatment.
- Seeing signs of soft tissue inflammation is crucial in understanding the extent of any related conditions or complications.
Can a blood test detect arthritis?
While there isn’t a specific blood test designed to detect it directly, in cases where your healthcare provider suspects gout or rheumatoid arthritis, they might request blood work.
This examination aims to identify the presence of uric acid or inflammatory proteins in your blood, which can provide valuable insights into the potential existence and type of arthritis you may be experiencing.
How is arthritis treated?
Arthritis, unfortunately, has no known cure, but various treatments are available to help you effectively manage the condition. The treatment plan will be tailored to your it’s severity, symptoms, and overall health condition.
Conservative, non-surgical treatments comprise several approaches, such as:
Medication
Anti-inflammatory and pain-relieving medications can provide relief from it’s symptoms. Biologics, a specific type of medication, target the immune system’s inflammatory response, and they may be recommended for conditions like rheumatoid or psoriatic arthritis.
Physical Therapy
Engaging in rehabilitation and physical therapy can significantly improve your strength, range of motion, and overall mobility. Therapists can also educate you on adapting daily activities to minimize arthritic pain.
Therapeutic Injections
Cortisone shots can temporarily relieve joint pain and inflammation. For specific joints like the knee, a treatment called visco-supplementation may be beneficial, involving lubricant injection to facilitate smooth joint movement.
Will I need surgery for arthritis?
In most instances, healthcare providers reserve surgical intervention for severe cases of it when conservative treatments have not yielded sufficient improvement. Surgical options may be considered in such cases and include
Fusion
This procedure involves permanently fusing two or more bones. By immobilizing the joint, fusion can effectively alleviate pain caused by movement.
Joint replacement
In this surgical approach, a damaged and arthritic joint is replaced with an artificial joint, preserving joint function and movement. Common examples of joint replacement surgeries include ankle, hip, knee, and shoulder replacement.
How can arthritis be prevented?
To reduce your risk of developing arthritis, you can take the following steps:
- Steer clear of tobacco products to protect your joint health.
- Engage in low-impact exercises that do not put excessive weight on your joints.
- Maintain a healthy body weight to alleviate strain on your joints.
- Take precautions to minimize the risk of joint injuries and preserve joint function.
What’s the outlook for someone living with arthritis?
Given that arthritis has no cure, individuals usually need to manage the condition throughout their lives. Your healthcare provider can assist you in finding the most practical combination of treatments to alleviate symptoms.
An essential aspect of it’s management is maintaining an active lifestyle. Inactivity resulting from joint pain can increase the risk of various severe conditions, including cancer, heart disease, diabetes, and others. You can help reduce these health risks and improve your overall well-being by staying physically active.
What can I do to make living with arthritis easier?
Making simple changes to your daily routine can significantly improve the experience of living with arthritis. Modifying your activities to reduce joint pain can be beneficial.
Collaborating with an occupational therapist (OT), a specialized healthcare provider in managing physical challenges like arthritis, can be advantageous.
An OT might suggest:
- Employing adaptive equipment like jar grips to make tasks like opening jars easier.
- Providing techniques to engage in hobbies, sports, or other activities safely, tailored to your needs.
- Offering valuable advice to minimize joint pain during arthritic flare-ups, enabling you to better cope with these episodes.
Do certain types of weather make arthritis worse?
For some individuals, arthritis symptoms may worsen under specific weather conditions. Humidity and cold temperatures are two common sources of joint discomfort.
Various factors contribute to this phenomenon. During rainy seasons and winter, people tend to be less active, which can impact arthritis discomfort. Cold and damp weather can also lead to joint stiffness and aggravate the symptoms.
Some theories propose that variations in barometric pressure, which measures air pressure surrounding us, could affect it’s symptoms.
If certain weather conditions exacerbate your arthritis, consider discussing effective symptom management strategies with your healthcare provider.
Simple measures like dressing warmly, engaging in indoor exercises, or utilizing heat therapy may relieve your pain.
Conclusion
Arthritis is a condition that impacts the joints, encompassing numerous types that lead to pain and decreased mobility. While some forms arise from natural joint wear and tear, others result from autoimmune or inflammatory conditions.
Managing it involves a range of treatments, including physical or occupational therapy and, in some cases, joint surgery.
Your healthcare provider will evaluate your symptoms and tailor a suitable treatment plan to address your needs. With effective management, most individuals can continue to engage in the activities they cherish despite having arthritis.