Receiving a diagnosis of breast cancer can elicit a mix of emotions. Gathering the necessary information to make informed decisions about your treatment plan can empower you during this challenging time.
If surgery is viable, you will encounter one of your initial significant choices: selecting the most suitable type. Understanding the critical details about commonly performed breast cancer surgeries is essential. Your doctor will guide you in determining the optimal choice tailored to your needs.
What Are the Different Types of Surgery?
In breast cancer treatment, there are two primary types of surgeries commonly employed:
Mastectomy
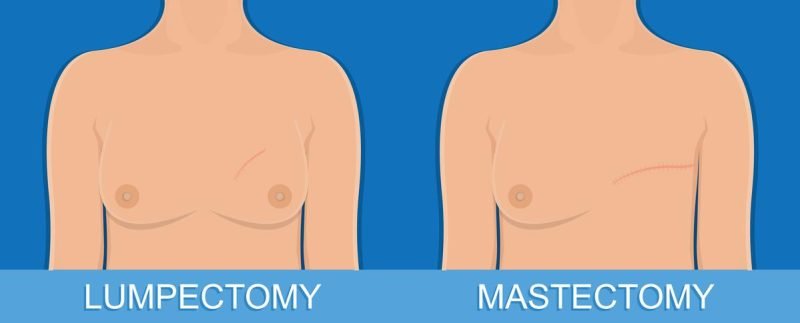
A simple mastectomy involves the removal of the entire breast and potentially a few lymph nodes in the armpit region. In the case of a modified radical mastectomy, the whole breast is excised along with the lymph nodes in the armpit area.
Lumpectomy
In this procedure, the surgeon removes the breast portion where the cancer is located, along with a border of healthy tissue surrounding the tumor and some nearby lymph nodes.
Lumpectomy aims to conserve as much breast tissue as possible and is often followed by radiation therapy to reduce the risk of cancer recurrence in the breast.
How Do I Decide Which Surgery to Get?
If you have been diagnosed with early invasive or locally advanced breast cancer, your doctor will likely recommend prompt surgery. Early-stage cancer patients may have the option of lumpectomy, also known as breast-conserving surgery, where only the affected portion of the breast is removed.
However, a mastectomy is usually the recommended course of action for locally advanced breast cancer, which carries higher risks. Research indicates that when radiation therapy is combined with lumpectomy, survival outcomes are comparable to those of mastectomy.
Chemotherapy has become the primary treatment method for women whose breast cancer has spread beyond the breast. Surgery for advanced cancer patients may be considered to alleviate symptoms, but it is not the primary treatment.
Mastectomy might be preferred in the following situations:
- If the breast cancer mass is significant.
- If you have small breasts and cancer is present in multiple areas of your breast.
- If the tumor is located under your nipple.
- If you are unable to undergo radiation therapy.
- If you are at higher risk of radiation side effects due to a connective tissue disorder like lupus or scleroderma.
- If you have previously received radiation therapy to the breast.
- If you are pregnant and radiation therapy during pregnancy could harm the baby.
If you opt for a mastectomy, you may also consider breast reconstruction surgery to restore the shape of your breast. Reconstruction can be performed simultaneously with the mastectomy or at a later time.
In some cases, women who undergo lumpectomy can have fat tissue transplanted from other body areas to help conceal any dimples resulting from the surgery.
In rare cases of male breast cancer, approximately 98% of patients receive a mastectomy as part of their treatment.
Does My Type of Surgery Determine My Life Expectancy?
Research indicates that your choice between lumpectomy followed by radiation or mastectomy does not significantly impact your overall lifespan.
Both types of surgery carry a small risk of cancer recurrence. Within 12 years, approximately 5% to 10% of women who undergo breast-sparing surgery followed by radiation may experience a recurrence of cancer in the same breast. In such cases, a mastectomy becomes a viable option.
For women who opt for a mastectomy, the risk of cancer recurrence on the same side of the chest within 12 years is slightly lower, around 5%.
It’s important to note that breast reconstruction surgery does not increase the risk of developing cancer in the operated breast and has no impact on life expectancy.
What Should I Expect After Surgery?
Pain is joint after surgery, and discussing pain management options with your doctor before the procedure is essential. Recovery times vary depending on the type of surgery you undergo. If you have a lumpectomy, you can expect to resume everyday activities within 5 to 10 days.
For a mastectomy, it may take 3 to 4 weeks to start feeling back to normal, and if breast reconstruction was also performed, the recovery time could be extended to 6 to 8 weeks.
Following a lumpectomy or other breast-sparing surgery, your breast should resemble its appearance before the operation, and you should retain feeling in your breast, nipple, and areola.
However, if you underwent the removal of a prominent cancer, your breast may appear smaller or different, and a small scar will be present where the tumor was removed.
After a mastectomy, the breast and nipple will be removed, leaving a flat surface on the operated side of your chest. If your breast is large, the scar may be longer compared to that of a smaller-breasted woman.
It’s common to experience numbness in the skin where the breast was removed and possibly under the arm.
While some sensations may return within a year or two, it may not be the same as before the surgery. In breast reconstruction cases, feeling in most areas around the breast will be diminished.
What Are the Risks of Complications?
Every surgical procedure carries inherent risks; lumpectomy and mastectomy are no exceptions. The most common complications associated with both surgeries are similar and may include:
- Pain
- Infection
- Bleeding
- Swelling
Since mastectomy is a more extensive and invasive procedure, the risks of experiencing these complications are comparatively higher.
Will I Need More Treatment?
Following the surgery, additional treatments are often necessary. Radiation therapy is usually prescribed for patients who undergo a lumpectomy or other breast-conserving surgeries, typically administered five days a week for 1 to 6 weeks. Even if you choose a mastectomy, radiation therapy may still be recommended.
In addition to surgery and radiation, your treatment plan might include chemotherapy, hormone therapy, or targeted therapy, depending on your specific case and the type of breast cancer you have.
It’s important to note that even after a lumpectomy, further surgery may be required to eliminate any remaining cancer cells. Likewise, with mastectomy, additional surgeries might be necessary.
It is common for patients to undergo more than one surgery after breast reconstruction to achieve the desired outcome.
What Other Considerations Affect Breast Cancer Surgery Selection?
When choosing between a lumpectomy and mastectomy, various factors should be considered, including potential complications, recovery time, and personal preferences regarding breast appearance.
Financial considerations might also play a role in your decision, as breast cancer treatment costs can vary significantly, encompassing hospitalization and follow-up care.
Surprisingly, research indicates that only 22% of women discuss the cost of their surgery with their medical team, and about one-third of women find that their care costs more than expected.
Even if you have insurance, addressing costs upfront is essential to make informed decisions. If available, inquire if your treatment center has a “financial navigator” or a similar professional to discuss costs with you.
Moreover, a woman’s race or ethnicity might influence her choice between mastectomy and lumpectomy. A study published in Annals of Surgical Oncology revealed that 41% of American Indian and Alaska Native women with early-stage breast cancer opted for a mastectomy, compared to 34% of white women.
Conversely, a higher percentage of white women (65.6%) chose lumpectomy than 59% of Indigenous women.
It’s crucial to remember that if lumpectomy is a suitable option, selecting a mastectomy won’t increase your chances of living longer. Additionally, research indicates that mastectomy may be more costly and carry a higher risk of complications.